The future of disease tracking is going down the drain — literally. Flushed with success over detecting coronavirus in wastewater, and even specific variants of SARS-CoV-2, the virus that causes COVID-19, researchers are now eyeing our collective poop to monitor a wide variety of health threats.
Before the pandemic, wastewater surveillance was a smaller field, primarily focused on testing for drugs or mapping microbial ecosystems. But these researchers were tracking specific health threats in specific places — opioids in parts of Arizona, polio in Israel — and hadn’t quite realized the potential for national or global public health.
Then COVID-19 hit.
The pandemic triggered an “incredible acceleration” of wastewater science, says Adam Gushgari, an environmental engineer who before 2020 worked on testing wastewater for opioids. He now develops a range of wastewater surveillance projects for Eurofins Scientific, a global laboratory testing and research company headquartered in Luxembourg.
A subfield that was once a few handfuls of specialists has grown into more than enough scientists to pack a stadium, he says. And they come from a wide variety of fields — environmental science, analytical chemistry, microbiology, epidemiology and more — all collaborating to track the coronavirus, interpret the data and communicate results to the public. With other methods of monitoring COVID-19 on the decline, wastewater surveillance has become one of health experts’ primary sources for spotting new surges.
Hundreds of wastewater treatment plants across the United States are now part of COVID-19 testing programs, sending their data to the National Wastewater Surveillance System, or NWSS, a monitoring program launched in fall 2020 by the U.S. Centers for Disease Control and Prevention. Hundreds more such testing programs have launched globally, as tracked by the COVIDPoops19 dashboard run by researchers at the University of California, Merced.
In the last year, wastewater scientists have started to consider what else could be tracked through this new infrastructure. They’re looking at seasonal diseases like the flu, recently emerging diseases like bird flu and mpox, formerly called monkeypox, as well as drug-resistant pathogens like the fungus Candida auris. The scientists are even considering how to identify entirely new threats.
Wastewater surveillance will have health impacts “far broader than COVID,” predicts Amy Kirby, a health scientist at the CDC who leads NWSS.
But there are challenges getting from promise to possible. So far, such sewage surveillance has been mostly a proof of concept, confirming data from other tracking systems. Experts are still determining how data from our poop can actually inform policy; that’s true even for COVID-19, now the poster child for this monitoring. And they face public officials wary of its value and questions over whether, now that COVID-19 health emergencies have ended, the pipeline of funding will be cut off.
This monitoring will hopefully become “one of the technologies that really evolves post-pandemic to be here to stay,” says Mariana Matus, cofounder of Biobot Analytics, a company based in Cambridge, Mass., that has tested sewage for the CDC and many other health agencies. But for that to happen, the technology needs continued buy-in from governments, research institutions and the public, Matus and other scientists say.
How wastewater testing works
Wastewater-based epidemiology has a long history, tracing back at least to physician John Snow’s 1850s observations that cholera outbreaks in London were connected to contaminated water.
In the 1920s and ’30s, scientists began to take samples from sewage and study them in the lab, learning to isolate specific pathogens that cause disease. These early researchers focused on diseases that spread through contaminated water, such as polio and typhoid.
Today, automated machines typically retrieve sewage samples. The machines used to collect waste beneath maintenance hole covers are “like R2-D2 in terms of size” or smaller, says Erin Driver, an environmental engineer at Arizona State University in Tempe who works on collection methods.
Driver can plug this machine, or a larger version used for sampling at wastewater treatment plants, into a water pipe and program it to pull a small amount of sewage into an empty bottle at regular intervals, say, once an hour for 24 hours. She and colleagues are developing smaller versions of the automated sampler that could be better suited for more targeted sampling.
What happens in the lab to that bottle of waste depends on what scientists are testing for. To test for opioids and other chemicals, scientists might filter large particles out of the sample with a vacuum system, extract the specific chemicals that they want to test, then run the results through a spectrometer, an instrument that measures chemical concentrations by analyzing the light the chemicals give off.
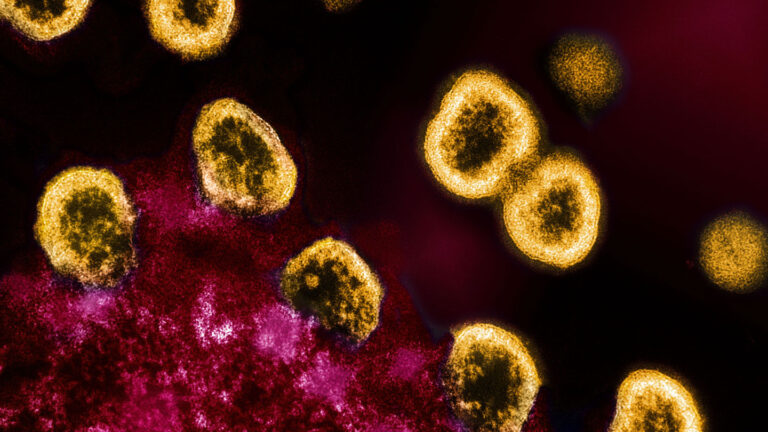
To determine levels of SARS-CoV-2 or another virus, a scientist might separate liquid waste from solid waste with a centrifuge, isolate viral genetic material, and then test the results with a PCR machine, similar to testing someone’s nose swab. Or, if scientists want to know which SARS-CoV-2 variants are present, they can put the material through a machine that identifies a variety of genetic sequences.
Would the coronavirus even show up in waste?
In the panicked early days of the pandemic, an urgent basic question loomed. “Will this even work?” remembers Marlene Wolfe, an environmental microbiologist at Emory University in Atlanta. While polio is spread through fecal matter, there were early hints that the coronavirus mostly spreads through the air; scientists initially weren’t even sure that it would show up in sewage.
On the same day in 2020 that the San Francisco Bay Area went on lockdown, Wolfe and colleagues at Stanford University, where she was based at the time, got a grant to find out. The team was soon spending hours driving around the Bay Area to collect sewage samples, “navigating lockdown rules” and negotiating special permissions to use lab space, she says.
“We were anxiously waiting to see if our first samples would show a positive result for SARS-CoV-2,” Wolfe says.
Not only did the sewage samples test positive, Wolfe and her colleagues found that coronavirus levels in the Bay Area’s wastewater followed the same trends as reported cases, the team reported in December 2020 in Environmental Science & Technology. When case counts went up, more virus appeared in the sewage, and vice versa. Early projects in other parts of the country showed similar results.
More than three years later, data on reported cases have become much less reliable. Fewer people are seeking out lab-based PCR tests in favor of easier-to-access at-home tests — with results often not reported. Wastewater trends have become the best proxy to provide early warnings of potential new COVID-19 surges, such as the increased spread this summer, to health officials and the public alike.
Opening the tracking floodgates
In summer 2022, wastewater tracking got a new chance to prove itself. Mpox was rapidly spreading globally, including in the United States. But tests were limited, and the disease, which was spreading primarily through intimate contact between men, quickly drew social stigma, leading some people to hesitate in seeking medical care.
Within a few weeks of the start of the U.S. outbreak, Wolfe and her colleagues, as well as research teams at Biobot and other companies, had developed tests to identify mpox in sewage.
Just as scientists had seen with COVID-19, mpox trends in wastewater matched trends in official case numbers. In California, wastewater results even suggested that the disease may have spread farther than data from doctors’ offices suggested, Wolfe and collaborators reported in February in the New England Journal of Medicine.
Like COVID-19, mpox doesn’t transmit through the water, but sewage testing still picked up the virus. The early results from that summer outbreak convinced some health officials that wastewater technology could be used for many diseases, no matter how they spread, Matus says.

Scientists are starting to find more and more infectious diseases that can be tracked in sewage. “Honestly, everything that we’ve tried so far has worked,” says Wolfe, who is now a principal investigator of WastewaterSCAN, a national sewage testing project led by researchers at Stanford and Emory. The project team currently tests samples for six different viruses and is working on other tests that it can send out to the more than 150 sites in its monitoring network.
Through an informal literature review of pathogens important for public health, scientists at Biobot found that previous research had identified 76 out of 80 of them in wastewater, stool or urine, suggesting that those pathogens could be monitored through sewage. The list ranges from the chicken pox virus to the microbes that cause sexually transmitted diseases like chlamydia to the tickborne bacteria that cause Lyme disease.
Finding focus
With this much opportunity, the question on many researchers’ minds is not, “What can we test for?” but “What should we test for?”
In January, a report put out by the National Academies of Sciences, Engineering and Medicine came up with three criteria. The pathogen should threaten public health. It should be detectable in wastewater. And it should generate data that public health agencies can use to protect their communities.
Given all the threats and hints of what can be found in wastewater, the first two criteria don’t narrow the field too much. So for now, researchers are taking cues from state and local public health officials on which pathogens to prioritize.
Biobot is working on tests for common diseases like the flu, RSV, hepatitis C and gonorrhea. And the CDC has its eye on some of the same common pathogens, as well as strategies for tracking antimicrobial resistance, a threat that has increased during the pandemic as health systems have been under strain.
Even if they choose the perfect targets, though, researchers also have to figure out how to generate useful data. For now, that’s a sticking point.
How to use the data
Tracking pathogens is one thing. But determining how the results correspond to actual numbers of sick people is another, even in the case of COVID-19, where researchers now have years of detailed data. As a result, many public health officials aren’t yet ready to make policy decisions based on poop data.
In New York City over the last three years, for example, the local government has poured more than $1 million into testing for COVID-19, mpox and polio in sewage from the city’s water treatment plants. But the city’s health department hasn’t been using the resulting data to inform local COVID-19 safety measures, so it’s unclear what’s being done with the data.
Health officials are used to one swab per person, says Rachel Poretsky, a microbiologist at the University of Illinois Chicago. She also heads wastewater monitoring for the city of Chicago and the state of Illinois.
Public health training relies on identifying individual sick people and tracing how they became ill. But in wastewater surveillance, one data point could represent thousands of sick people — and the data come from the environment, rather than from hospitals and health clinics. What to do next when positive results turn up isn’t as obvious.
Numbers collected from the health care system always represent patients, so a spike indicates a surge in cases. In the case of sewage data, however, environmental factors like weather, local industries and the coming and going of tourists also can create “weird outliers” that resist easy interpretation, Poretsky says. For instance, a massive rainstorm might dilute samples, or chemical runoff from a factory might interfere with a research team’s analytical methods.
Data interpretation only gets more complicated when scientists begin testing wastewater for an increasing number of health threats. Every pathogen’s data need to be interpreted differently.
With coronavirus data, for example, wastewater tests consistently come back positive, so interpreting the data is all about looking for trends: Are viral concentrations going up or down? How does the amount of virus present compare with the past? A spike in a particular location might signal a surge in the community that hasn’t yet been picked up by the health care system. The community might respond by boosting health resources, such as opening vaccine clinics, handing out free masks and at-home tests, or adding staff to local hospital emergency departments.
Mpox, on the other hand, has infected far fewer people, and positive tests have been rare after last summer’s outbreaks ended. Now, researchers are simply watching to see whether the virus is present or absent in a given sewershed.
“It’s more about having an early warning,” Matus says. If a sewershed suddenly tests positive for mpox after negative results for the last few months, health officials might alert local doctors and community organizations to look out for anyone with symptoms, aiming to identify any cases and prevent a potential outbreak.
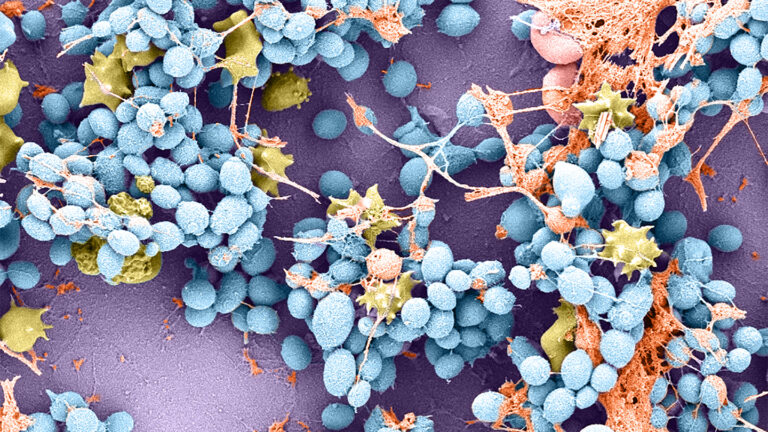
Another complicated pathogen is C. auris, a fungus that has developed resistance to common drugs. It can spread rapidly in health care settings — and be detected in sewage. Researchers from Utah and Nevada reported in February in Emerging Infectious Diseases that it was possible to track C. auris in the sewage from areas experiencing outbreaks.
If hospitals or health officials could identify the presence of this fungus early, that information could guide public health actions to curb outbreaks, says Alessandro Rossi, a microbiologist at the Utah Public Health Laboratory in Salt Lake City. But interpreting the warnings isn’t as clear-cut for C. auris as for viruses.
The fungus can grow in sewage after it leaves health care facilities, Rossi says. The pathogen has “the potential to replicate, form biofilms and colonize a sewershed.” In other words, C. auris can create its own data interference, potentially making wastewater results seem worse than they really are.
Moving wastewater into the future
Most current testing programs are reactive. By looking at health threats one at a time using specific PCR tests, the programs mostly confirm that pathogens we already are worrying about are getting people sick.
But some scientists, like Wim Meijer, envision a future in which wastewater monitoring wades into the unknown and alerts us to unusual disease outbreaks. The microbiologist, of the University College Dublin, heads Ireland’s wastewater surveillance program. Ideally, in this ahead-of-the-curve future, after detecting something alarming in sewage, his team could closely collaborate with health officials to study the pathogen and, if necessary, start combating the threat.
One idea for turning the tech proactive is to prepare for new health threats that we can see coming. For example, Meijer and his colleagues are interested in screening Ireland’s sewage for the H5N1 bird flu, but they are not yet doing this testing.
Another approach takes advantage of genetic testing technology to look at everything in our waste. Kartik Chandran, an environmental engineer at Columbia University who has mapped sewers’ microbial ecosystems with this technique, describes it as “trying to shine the light more broadly” rather than looking where the light is already shining brightest.
Such an approach might identify new pathogens before sick people start going to the doctor’s office, potentially leading to an earlier public health response. But with health officials still unsure of how best to use wastewater data, much more basic research is needed first.

“People think wastewater surveillance is the answer to everything, and clearly that’s not true,” says Kirby, of the CDC, reflecting concerns from the state and local officials that she collaborates with at NWSS. Before diving ahead into proactive surveillance, Kirby and her colleagues are working to set up basic wastewater standards and protocols for health agencies. Priorities include evaluating how sewage trends correlate to cases for different pathogens and developing standards for how to use the data.
The wastewater surveillance field also needs to keep growing if the goal is to monitor and contribute to global health, with more sites contributing data and more scientists to analyze it. All of this work requires sustained funding.
The CDC’s program so far has been funded by COVID-era legislation and will run out of money in 2025. While wastewater surveillance is more cost-effective than other types of testing, it still requires a lot of resources. Washington’s state health department, for example, paid Biobot more than $500,000 for a one-year sewage testing contract, while the CDC has paid the company more than $23 million since 2020 for its work with NWSS.
For the last few years, wastewater surveillance has been a giant, messy group project. Scientists have collaborated across fields and locations, across private and public institutions, through Zoom calls and through poop samples shipped on ice. They’ve shown that waste might hold the key to a new way of tracking our collective health.
A lot of unanswered questions remain, and it could be some time before your local sewer can tell you exactly what disease risks you might be facing. But COVID-19 pushed thousands of experts to look into their toilets and start asking those questions. “Now, everyone’s a believer,” says Driver, of ASU. “Everyone’s doing the work.”





+ There are no comments
Add yours