
Electricity Saved My Brain
This is the second part in a series on deep brain stimulation for depression. Read from the beginning.
[Content note: This story contains discussion of suicide.]
Jon Nelson’s depression was poison. “I had poison in every single bit of my body. It literally ran throughout every cell in my body. My blood carried the poison, and it crushed everything in me.”
Melancholia, one of depression’s early names, comes from the ancient Greek word for “black bile,” a diseased liquid believed to flood a body. It was once thought that bloodletting and other ways to let the corrupting fluids out could ease people’s minds.
Today, doctors have much better options to treat depression. Antidepressant drugs and talk therapy can be effective for many people. But these options don’t help everyone.
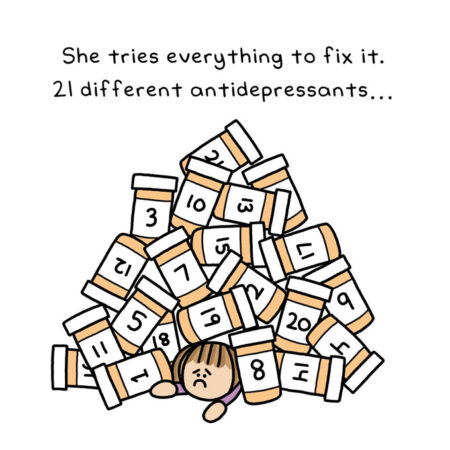
Jon has treatment-resistant depression. So does Amanda, an app and web designer and artist in her 30s who lives in New York City. Amanda can also rattle off a long list of therapies she has tried for the deep depression she’s felt since she was 13. She has been on 21 different antidepressant drugs. Her brain has been zapped with powerful magnets in a therapy called transcranial magnetic stimulation. She has had IV infusions of ketamine.
Amanda, who to protect her privacy requested her last name not be used, has also had 40 rounds of electroconvulsive therapy, or ECT. The “gold standard” treatment for people who aren’t helped by other therapies, ECT is often done several times a week for three or four weeks. For unknown reasons, the resulting mini-seizures in the brain can sometimes provide relief.
“The electroconvulsive therapy helped a little bit,” Amanda says. “But for it to help, I had to do it so frequently that I got memory damage. I was like, ‘Whoa, whoa, whoa, I don’t remember where my sock drawer is. I don’t remember what subway stations are near my apartment. I don’t remember how to use the software I’ve been using for 10 years,’” she told me. “I have to stop.”
Jon’s depression was poison; Amanda’s was a vortex. And when ECT was no longer an option, that vortex nearly consumed her. After a suicide attempt, she spent six weeks in the hospital and then another six weeks receiving outpatient care. “It was at that point that [doctors] were like, ‘There’s nothing else we can do for you. You’ve tried literally everything that’s out there. If ECT doesn’t work, that’s it,’” Amanda says.
As with Jon and others I talked with, her doctors had given up, Amanda says. “When you get to that place where they say there’s nothing else we can do for you, and yet you have to keep living your life, that’s a hard place to get to.”
The last hope
Desperate for help, Amanda called the treatment-resistant depression program at Mount Sinai. After describing all of her unsuccessful treatments, Amanda was once again passed along to different doctors. “They had decided that you really have tried everything,” she says.
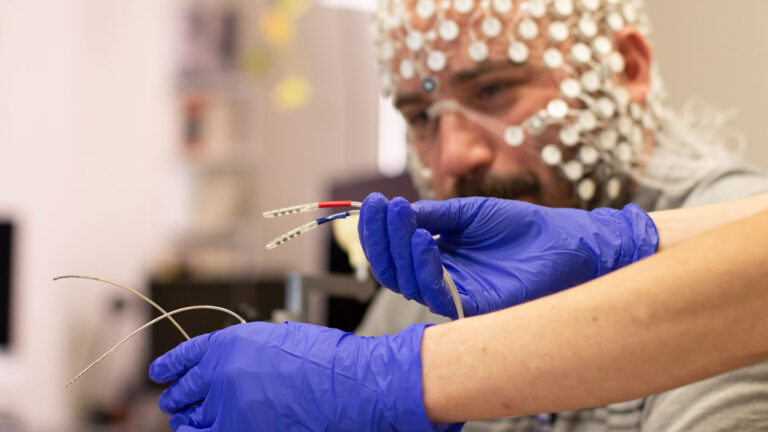
That last handoff is what delivered Amanda to the DBS research program. As Martijn Figee, a psychiatrist and DBS researcher at the Icahn School of Medicine at Mount Sinai, explained the procedure, the research and the risks, Amanda listened carefully. She arrived at appointments prepared with an eight-page-long list of questions that covered the practical (“What should I avoid forever once I have it? Running? Hanging my head upside down? Trampolines?”) and the profound (“What makes a person want to be alive?”). Questions answered and fully informed, Amanda agreed to have DBS surgery.
The DBS program that Amanda and Jon are a part of looks vastly different from earlier iterations. In 2008, neurologist Helen Mayberg and many colleagues around the country had just begun a large, double-blind DBS clinical trial to test the technique. Called the Broaden trial, the six-month study followed people with depression, some of whom had electrical stimulation on and others who were implanted with electrodes but had the stimulation off.
All told, 90 people with severe depression were implanted with brain stimulation devices in the trial. But in 2013, testing stopped early because of poorer-than-expected results. The sponsor and maker of the DBS device, St. Jude Medical Inc., determined that the trial wasn’t likely to hit its goals. Along with another unsuccessful trial, which included 30 people who received stimulation in a different part of the brain, those lackluster results represented a real setback for DBS as a treatment for depression.
Those disappointing findings fueled criticisms of the method, underscored by stories of people who had negative experiences with DBS. And potential conflicts of interest exist, as they do for many medical treatments that depend on medical device companies. Mayberg, for instance, receives fees for consulting and licensing intellectual property from Abbott Laboratories, the company that bought St. Jude Medical.
Despite setbacks and criticism though, the research didn’t stop; it matured. Brain-imaging methods got better, allowing researchers to see exactly which highways of white matter fibers, message-sending bundles that emanate from nerve cells, are influenced by the electrodes. Other aspects of care, including follow-up sessions with mental health experts and therapists, have evolved. In a small trial of 11 people with severe depression, for instance, nine had their symptoms improve, researchers reported in 2018. And DBS as a depression treatment has been able to borrow heavily from progress in treating other disorders.
How widespread is DBS?
Globally, DBS electrodes have been implanted in an estimated 230,000 people’s brains. DBS was approved by the U.S. Food and Drug Administration in 1997 to treat tremor, and in 2002 to treat Parkinson’s disease. DBS is also used by doctors for severe cases of epilepsy, obsessive-compulsive disorder and dystonia, or involuntary muscle contractions.
DBS’s reach is expanding fast. In smaller experimental trials, people have been implanted with electrodes for pain, eating disorders, addiction, traumatic brain injuries and post-traumatic stress disorder. Researchers are working on stimulation systems to restore movement to paralyzed people and speech to people unable to talk.
Jon heard about the procedure in 2021. He called the Mount Sinai program from a residential treatment facility, only to learn that he didn’t qualify because, at the time, he hadn’t yet tried ECT. So he did 12 rounds of the therapy in early 2022. ECT helps many people. But it didn’t help Jon, and the experience shook him. “It was horrific. Zero relief. My memory loss is still pervasive to this day,” he says. It was utter misery, but he qualified for the DBS trial.
And with that, Jon’s surgery date was set: August 22, 2022.
In the run-up to the surgery, Jon’s wife, Barbara, worried about both the surgery and the outcome. “What if they slip or they sneeze and they ruin his brain?” she recalls wondering. “What if it doesn’t work? What do we do next? This was so much like the last resort that if it didn’t work, then we were going to be looking at potentially years more of trying.”
She adds, “And there’s no option of giving up.”
Even so, Barbara didn’t fully believe the surgery was going to happen until it was right around the corner. “I think my brain just did not catch up to the reality of it until we were very close to the actual surgery,” she told me. “A couple of days before, I was like, ‘Oh I’m a mess.’ I do weird things when I’m really that stressed out, rearranging furniture, doing things that seem to take too much energy.”
Jon, however, was not worried. “I didn’t care that I was having my head cut open,” he says. “I had the same level of anxiety that you would have if you were getting your teeth cleaned.”
If you or someone you know is facing a suicidal crisis or emotional distress, call or text the 988 Suicide & Crisis Lifeline at 988.
In the next article in the series, read about Jon’s surgery and the big changes that followed for him and his family.
This series was made possible with funding from the Alfred P. Sloan Foundation.





+ There are no comments
Add yours