Neurologist Helen Mayberg cringes at the slow pace of DBS research. Her first paper describing DBS for depression in the subcallosal cingulate (then called Brodmann Area 25) appeared in the journal Neuron in 2005. Almost 20 years later, she almost can’t believe that researchers are not further along in bringing this technique to people who would benefit from it.
“On the other hand, we’ve learned so much that maybe it’s not so bad,” Mayberg says. Still, she feels impatient. “We don’t have a lot of time,” she says. “People are dying now, so let’s fix them. And then we can make something better.”
Mayberg hopes to see the treatment become streamlined. The first heart pacemaker was an incredible piece of technology, but it was giant and clunky. Today, the powerful device, usually about the size of a matchbook, sits near millions of people’s hearts, keeping them beating. As with the heart, for the brain, “how do you go from complicated to simple? Everything is about the prototyping and the simplification,” she says.
What’s next? “What’s the future of this, the future three steps ahead?” Mayberg says. “I have no idea.”
Despite stories from Jon Nelson and others, deep brain stimulation still has its stigma to overcome, even in the research world. Questions of autonomy — of control over feelings and actions — crop up in ethics discussions of brain technology. But to Martijn Figee, the psychiatrist and DBS researcher who has worked with many people implanted with electrodes, those questions are a “luxury problem.” That framing ignores the idea that mental illness itself takes away a person’s control. “People who work in DBS are always a little frustrated by these discussions,” Figee says. “We’re always like, ‘Talk to the patients.’”
Figee, who receives consulting fees from Medtronic, a device company that makes brain implants, and his colleagues asked people before and after surgery for DBS for obsessive-compulsive disorder and Parkinson’s about their feelings of being in control of themselves. People did not report a loss of feeling in control of themselves after the procedure. In fact, the people treated for OCD reported a bigger jump in autonomy and control than the Parkinson’s patients. “That’s not something that bothered them at all,” Figee says, “because the OCD was more of a prison to them than the fact that they have this implant.”
Psychologist Shannon O’Neill, who treats people with DBS at Mount Sinai, says she hopes that the procedure will be more readily understood in the future: “What I’d love is a shift toward not making it a last resort,” she says. “I wonder if we wait too long to give an individual DBS.” She doesn’t mean that brain implants would be an early treatment, but instead, she wants other health care professionals to have more awareness of the procedure so that they can refer people who have run out of hope.
What are the open questions?
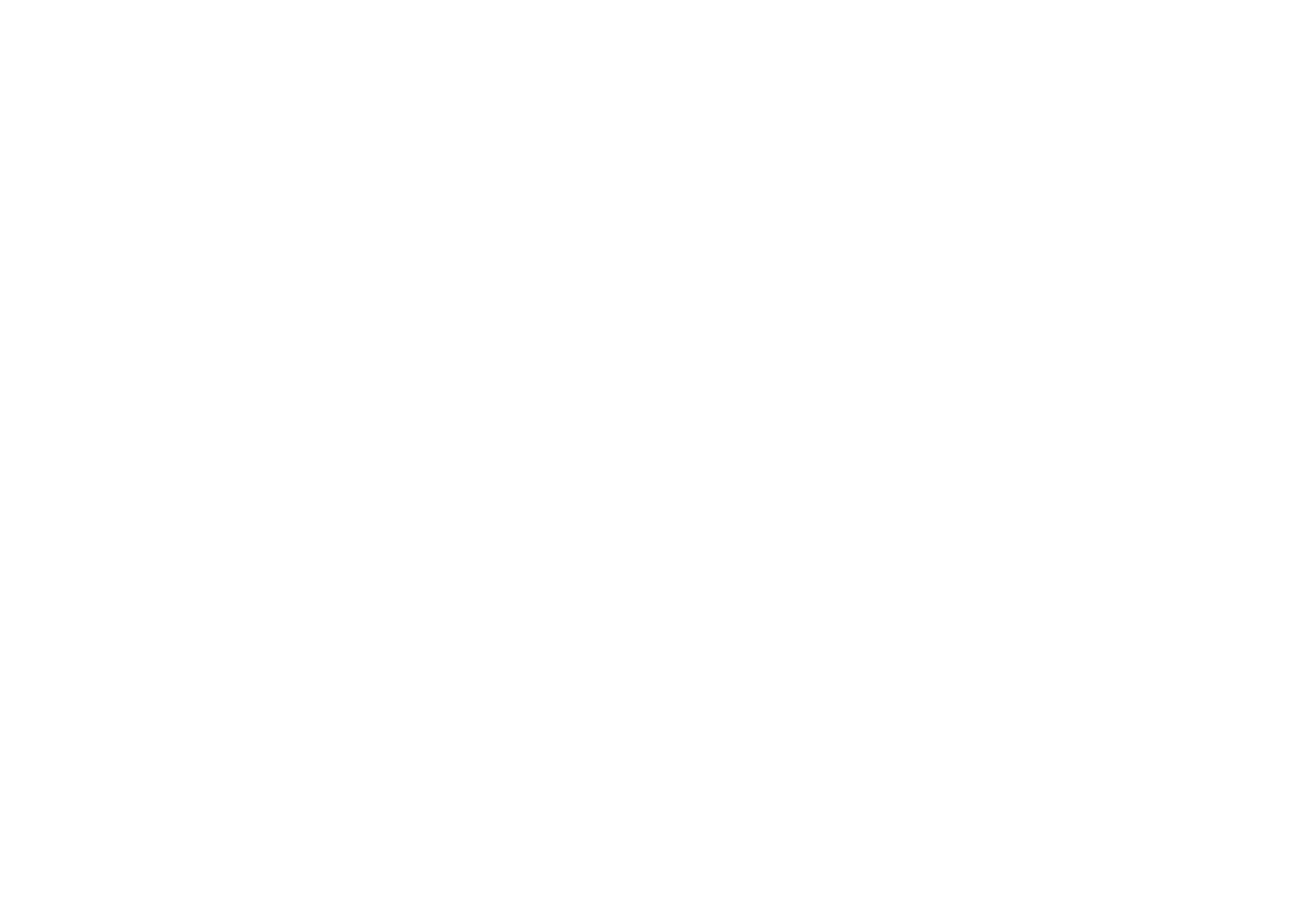
What’s next will almost certainly include nuanced and complex science. Big questions remain about where in the brain to stimulate, for which people and what kind of stimulation. Jon and Amanda are participating in follow-up studies searching for signs of recovery in their brains, bodies and microexpressions on their faces, and even in their voices. “The commitments are out of control,” Jon jokes. He spends eight minutes twice a day recording his brain waves, along with video journals and daily, weekly and monthly surveys. His brain is imaged regularly.
Researchers are searching for a hallmark, a signature, that can tell them the method is working. “I need to know when the depression is away, and I need to have a way to discriminate,” Mayberg says. “When are you having a bad day and when are you relapsing? Those are not the same thing.”
Mayberg and her colleagues just described one such hallmark in six people who underwent DBS for depression. A collection of changes in brain behavior can indicate when a person has recovered, the researchers reported September 20 in Nature.
A handful of trials are putting a spin on the typical DBS approach and studying what’s called adaptive DBS, which kicks in only when a certain pathological brain activity pattern is detected. That approach has worked well for a woman named Sarah with severe depression. Researchers at the University of California, San Francisco published the details of her improvements in 2021.
Similar on-demand efforts are happening for other disorders, including binge eating and post-traumatic stress disorder. Jay Gill, a brain researcher and medical student at UCLA told me that one man, a veteran with PTSD, described having an aura, a sort of premonition, just before his symptoms would get bad. With his adaptive DBS system in place, he still gets triggered and feels the aura, but instead of feeling worse, a feeling of calm sets in.
The optimal DBS approach for depression may be similar to the approach for PTSD, OCD, addiction and other psychiatric disorders. Or maybe not. There’s still so much to learn.
Not everyone thinks about depression, or any illness for that matter, as a battle. Jon does. And there were days — lots of days — when he thought he’d lose it.

These days, the Nelson house is bright. It’s full of laughter, riddles, good-natured teasing, homemade pizza — and an energetic kid on in-line skates who twirls and glides through the kitchen loop. It’s also full of hope for a future that’s better than the past. That makes me reluctant to ask Barbara a question that I know will be hard for her to answer: Is she worried that Jon’s DBS treatment will stop working?
“That’s always in the back of my mind a little bit,” she tells me. Over the years, Barbara has learned to temper her expectations for the future. “You just never really know what’s going to happen,” she says. In a way, she’s still guarded. “I don’t know if this is going to work forever,” she says.
“But my perspective is that even if something changes, we have had this time with him.… And if it keeps going forever, that’s amazing. It’s amazing. I hope it does.”
On the drives home from softball, field hockey, golf, basketball and ice hockey, Jon and whichever kids are around have chats. “I always call it ‘car talk with the kids.’” In one of these car talks, Jon’s youngest piped up. “He’s like, ‘Dad, I’m so happy you just kept fighting for us.’ These little comments that come out of nowhere. I’m like, ‘Oh my God. They get it. They understand it.’ It’s a trip.”
This series was made possible with funding from the Alfred P. Sloan Foundation.






+ There are no comments
Add yours