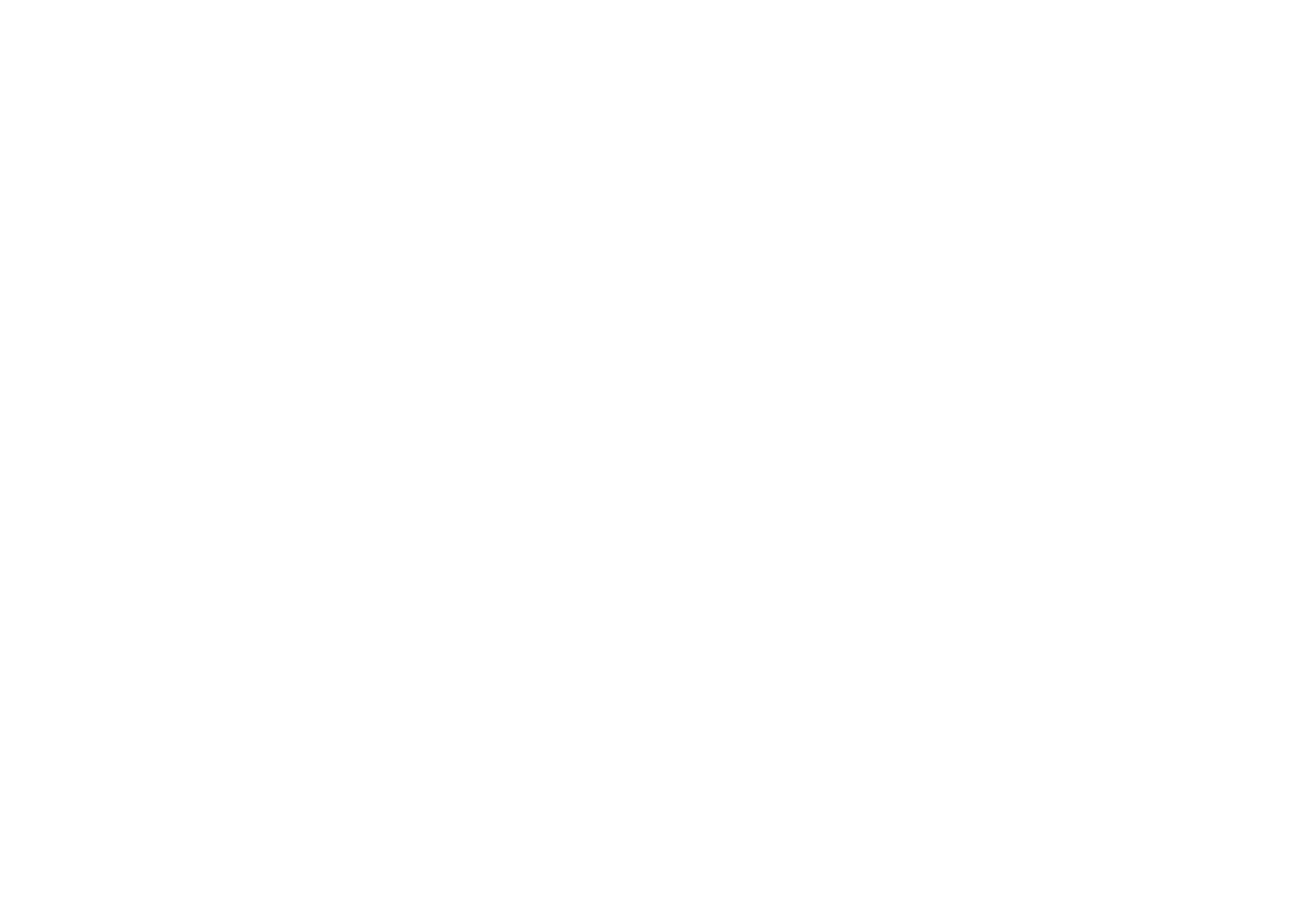
Candida auris, a fungus that causes sometimes deadly infections, can stick to almost any surface.
In hospitals, “it’s very tenacious, very difficult to get rid of and ends up on all the surfaces around patients,” where it can fuel outbreaks, says Darian Santana, a microbiologist at the University of Michigan Medical School in Ann Arbor. The fungus has been spreading rapidly since cases first emerged in several locations around the world in 2012 (SN: 3/20/23).
Santana and colleagues have discovered how the fungi stick to a wide variety of surfaces. Most fungi make adhesive proteins that rely on hydrophobic interactions to glom onto surfaces. Think oil and water, says Teresa O’Meara, a microbiologist and geneticist in whose lab Santana works. Oil droplets congregate with other oil droplets, while water is attracted to water. Similarly, hydrophobic fungal proteins attach themselves to hydrophobic, or water-repellent, surfaces.
C. auris has hydrophobic adhesion proteins too, but it mainly pastes itself to surfaces using electrical charges, the researchers report in the Sept. 29 Science. The fungus makes protein called SCF1, which contains many positively charged amino acids. The positive charge creates attraction with negative charges on surfaces, including skin and medical devices. It’s similar to the way barnacles stick to boats, Santana says.
The protein allowed the fungus to infect skin samples and colonize catheters in the lab, the team found. Without SCF1, the fungus was unable to spread in infected mice.
The finding may eventually lead to new ways to prevent or treat C. auris infections, O’Meara says. For instance, treatments may turn off production of the protein to prevent the fungus from spreading more widely in infected people, or a vaccine or antibody might stop the fungus from binding to surfaces and head off illness.









+ There are no comments
Add yours